Full Body Thermography
Thermography serves as a valuable tool and offers multiple applications for full body imaging. Thermography can help identify and monitor a wide range of diseases, functional imbalances, and physical injuries by revealing abnormal thermal patterns on the surface of the body. Because many conditions begin with inflammation, altered circulation, or nerve irritation—long before structural changes appear—thermography offers a unique advantage. It can visually display patterns of pain, dysfunction, or physiologic stress even when other tests, such as X-rays, MRIs, or ultrasounds, fail to pinpoint the cause. This makes it an invaluable option for individuals struggling with unexplained pain, unresolved symptoms, or chronic conditions that have been difficult to diagnose through conventional means.Full-body thermal imaging serves as an additional risk-free assessment tool that is completely non-invasive, contact-free, and free of radiation or harmful contrast dyes. The imaging process is simple and comfortable, making it suitable for individuals who require frequent monitoring or prefer not to undergo repeated exposure to ionizing radiation. By offering a broad, head-to-toe view of physiologic activity, full-body thermography can uncover hidden areas of inflammation, vascular compromise, lymphatic congestion, or musculoskeletal strain that may not yet be producing noticeable symptoms.Thermography can also help confirm or support diagnoses that patients may already be navigating. When used alongside traditional testing, it provides a deeper, more functional understanding of what the body is experiencing in real time—enhancing the ability to track progress, evaluate treatment effectiveness, and identify new or changing patterns over time.As explained by Dr. Lipton in the video below, thermography is fundamentally a test of physiology rather than anatomy. This distinction is critical: by detecting physiologic abnormalities and precursors to disease earlier in the process, thermography empowers individuals and clinicians to take proactive steps toward prevention, early intervention, and improved long-term health outcomes. This is key to being able to take preventative steps in fighting or preventing disease.

Autonomic thermal patterns are typically hypothermic, meaning they appear cooler on a thermogram compared to the surrounding tissue. These patterns can provide important clues about how the autonomic nervous system is functioning and may reveal early signs of organ stress or dysfunction. In some cases, hypothermic autonomic responses correspond to compromised circulation, nerve interference, or reduced metabolic activity within an organ system. For example, in patients with Coronary Artery Disease, thermography may show characteristic areas of cooling along specific autonomic pathways. These subtle temperature changes help clinicians recognize physiologic irregularities long before structural imaging reveals obvious abnormalities.
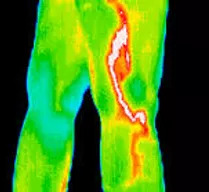
In this case, the patient’s phlebitis was not detected through conventional diagnostic tests, yet Digital Infrared Thermal Imaging (DITI) clearly revealed the issue. Because thermography measures subtle changes in heat and vascular activity, it can visually display inflammation, irritation, and circulatory distress long before they become apparent through structural imaging. Vascular pain, vein inflammation, and abnormalities in blood flow often create distinct thermal patterns that stand out on a thermogram. By capturing these temperature variations, DITI provides a valuable, non-invasive way to identify conditions like phlebitis earlier and more accurately, supporting timely follow-up and appropriate medical intervention.
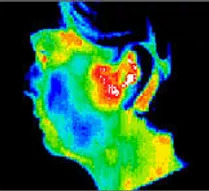
Temporomandibular joint (TMJ) disorders can be notoriously difficult to diagnose because symptoms often overlap with dental issues, nerve irritation, muscular tension, and even cervical spine problems. Thermography offers a unique advantage by visually displaying the combined effects of inflammation and neurological dysfunction in the jaw, face, and surrounding structures. Elevated heat patterns may indicate active inflammation, while areas of cooling can reflect nerve-related impairment or muscular imbalance. By mapping these physiologic changes, thermal imaging helps clinicians better understand the underlying contributors to TMJ pain, guiding more targeted treatment and providing insight when traditional diagnostic methods fail to pinpoint the true cause.
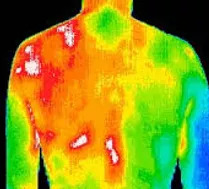
The muscular and myofascial inflammation associated with Fibromyalgia can be objectively documented and monitored through thermography. Because this condition often involves widespread pain, tender points, and fluctuating levels of inflammation, it can be challenging to assess using traditional diagnostic tools. Thermal imaging, however, captures subtle changes in heat distribution that correlate with muscle irritation, nerve sensitivity, and localized inflammatory responses. These patterns provide visual evidence of the patient’s symptoms, validating their experience while offering clinicians a clearer understanding of the areas most affected. Over time, thermography can also track improvements or flare-ups, making it a valuable tool for monitoring treatment effectiveness.
Frequently Asked Questions
- Can lifestyle changes (nutrition, sleep, stress reduction) affect my thermogram results — and how long after making changes would those effects show up?
- If the full-body scan shows an area of concern (e.g., increased heat in the abdomen or neck), what are the recommended next steps — and can the scan help track the effectiveness of my treatment plan?
- Is there any situation in which a full-body thermography scan might produce misleading results — and how should a client prepare or interpret the results to minimize false positives or negatives?
Q1. Can lifestyle changes (nutrition, sleep, stress reduction) affect my thermogram results — and how long after making changes would those effects show up?
A. Yes — because full-body thermography detects physiological changes (such as inflammation, vascular changes, lymphatic congestion) rather than just structural abnormalities, your body’s response to lifestyle shifts can influence subsequent scans. For example, improving sleep quality or reducing chronic stress may reduce autonomic dysfunction or neuro-inflammatory patterns; adopting an anti-inflammatory diet may reduce abnormal heat signatures. While individual results vary, clinics typically recommend waiting 3 to 6 months after major lifestyle adjustments to repeat a scan, so that your new baseline can be established and meaningful change can be observed. (Many practices initially use 90-day intervals to solidify a baseline for comparison.)
Q2. If the full-body scan shows an area of concern (e.g., increased heat in the abdomen or neck), what are the recommended next steps — and can the scan help track the effectiveness of my treatment plan?
A. When the scan reveals a “hot spot” or asymmetric thermal pattern, the next step is typically: (1) review the findings with your primary care physician or a specialist to correlate with other tests/exam findings, (2) use targeted diagnostics if indicated (e.g., ultrasound, MRI, blood work) to explore anatomy and function in that region, and (3) integrate corrective action (such as lifestyle interventions, therapies, or medical treatment). Yes — one of the benefits of full-body thermography is its ability to be used for monitoring: after treatment or lifestyle change, a follow-up scan can show whether the abnormal thermal pattern is resolving, stable, or worsening. This makes it a useful tool in a proactive health monitoring strategy.
Q3. Is there any situation in which a full-body thermography scan might produce misleading results — and how should a client prepare or interpret the results to minimize false positives or negatives?
A. Yes — several factors can influence scan accuracy and create misleading patterns: recent exercise, massage, heat or cold exposure, sunburn, use of creams/lotions, or even sitting positions prior to scan. To minimize false readings, clients should avoid heavy physical activity, hot tubs/saunas, and topical skin products for a specified period before the scan (often 24-48 hours). They should ensure the scanning facility follows strict protocols regarding room temperature acclimation, body positioning (e.g., standing vs sitting may matter) and that any recent treatments or surgeries are disclosed. Further, thermography is not a stand-alone diagnostic tool: it shows functional thermal changes, not definitive anatomical pathology. Therefore, results should be interpreted as part of a broader health assessment—ideally in conjunction with clinical exam and other imaging as needed.