2D Mammograms, Thermograms, 3D Mammograms, Ultrasounds, MRI's--which is the right choice?
It's time to understand the differences between all the available breast screenings and tests.
None of these tests are panaceas, which means none of these tests are complete solutions. Each test reveals a piece of the puzzle, a different perspective that when put together allows you and your doctor to have a more complete picture from which to understand your breasts' health.
Our purpose with this article is to help you understand each piece of the puzzle and how it may fit in to your picture. While we are thermography providers we do not claim that thermography is the only test you should have nor is this article purposed to convice you to have a thermogram. We do, of course, believe thermography is a valuable tool; but thermography, like mammography and other tests, has its pros and cons. Therefore what we hope to accomplish here is to give you an understanding of these pros and cons for each different test so that you can make an informed decision for yourself in conjunction with your medical doctor.
2D Mammograms
FDA Approved and recommended: mammograms are truly the main stream method used for breast screening. In fact, the FDA requires that providers first recommend the mammogram in most situations above any other test, subsequently approving thermography and other screenings only as 'adjunct' (in addition to) tests. Consequently, mammograms are usually referred to as 'The Golden Standard'.
Mammography, however, while the primary recommendation of the FDA, has its pros and its cons.
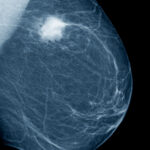
As shown in the image on the right a mammogram has identified a cancerous mass in white. This is by use of X-ray which allows the mammogram to identify abnormal structures or calcifications (1). In this regard, the mammogram is far superior to other tests: the mammogram is typically the only test that can show microcalcifications and as a test of structure can be more reliable than an ultrasound which is subject to the sonographer's skill.
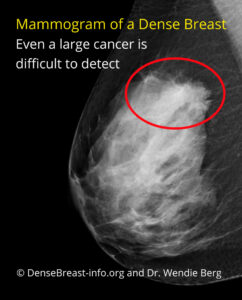
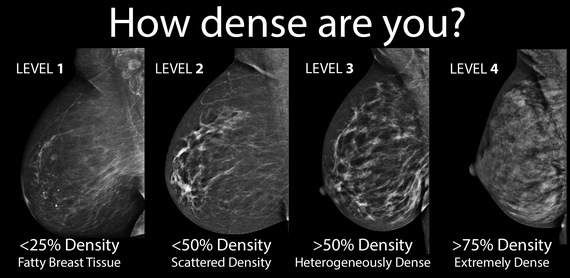
As seen above, if a mass is present in the breast a mammogram can detect it, but certainly is not garaunteed to. Dense breasts, one structure in front of a another (masking), and other issues can prevent a mammogram from detecting cancerous masses that are present.
Dense breasts are only an issue for mammograms. The accuracy of thermograms, ultrasounds, and MRI's are not affected by the density of breast tissue.
As seen in the picture to the left, dense breast tissue can make even large cancers difficult to detect. In fact, many states have passed laws in recent years requiring that this be explained that just because a mammogram does not detect cancer does not mean cancer is not present. These laws also require an explanation of how breast density impacts screenings and classifies the patient's density as seen below.
Whether your breasts are dense or a mammogram can see clearly through you, three major issues still exist that often frighten women away from having them: compression, radiation and being unable to see certain cancers.
Compression: As early as 1928, physicians were warned to handle "cancerous breasts with care— for fear of accidentally disseminating cells" and spreading cancer. Nevertheless, mammography entails tight and often painful compression of the breast, particularly in premenopausal women. This may lead to distant and lethal spread of malignant cells by rupturing small blood vessels in or around small, as yet undetected breast cancers (2).
Research has shown that the force of compression varies to as much as 4.4 pounds per square inch (psi) (3). Many woman complain of significant pain and tissue damage as a result of this much force.
Radiation: Mammogram radation is much more damaging than a chest X-ray. Mammograms use ionizing radiation at a relatively high dose, which can contribute to the mutations that can lead to breast cancer. You can get as much radiation from one mammogram as you would from 1,000 X-rays (4).

Dr. Samuel Epstein, one of the world's top cancer experts, has stated:
"The premenopausal breast is highly sensitive to radiation, each 1 rad exposure increasing breast cancer risk by about 1 percent, with a cumulative 10 percent risk for each breast over a decade's screening."
Cancers more difficult for mammograms to detect: In addition to breast density being an issue, there are some cancers mammograms simply cannot or usually cannot detect. These include inflammatory breast cancer (disease), invasive lobular cancer, any cancers located outside of the compression area such as arm pits, and cancers located just under the skin. These can be detected by other tests which is why no one method of screening should be used alone.
A few other issues...
- Women who have had mastectomies are recommended to NOT have mammograms due to lack of sufficient breast tissue. In such cases a thermogram can still be used to monitor for physiological changes indicative or returning cancer in the skin or chest wall.
- Generally women under 40 are not recommended to have a mammogram. Other screenings such as ultrasound are available to younger women and thermograms for the purpose of breast screening are available to women as young as 24.
Thermography
Breast thermography is a non invasive test of physiology. It is a valuable procedure for alerting your doctor to changes that can indicate early stage breast disease. The benefit of breast thermography is that it offers the opportunity of earlier detection of breast disease than has been possible through breast self examination, doctor examination or mammography alone.
Thermography can detect subtle physiologic changes that accompany breast pathology, whether it is cancer, fibrocystic disease, an infection or a vascular disease. Your doctor can then plan accordingly and lay out a careful program to further diagnose and/or monitor you during and after any treatment.
Digital infrared thermal imaging's role in breast health is to help in early detection and monitoring of abnormal physiology and the establishment of risk factors for the development or existence of pathology, whether benign or malignant. When used adjunctively with other procedures the best possible evaluation of breast health is made.
Unlike mammograms, thermograms are radiation free and without compression. In terms of physical harm from the procedure there is absolutely no risk whatsoever--thermograms are completely safe. This makes thermography an ideal addition to your breast screenings: thermography can do no harm while providing additional perspective. It is able to detect a number of conditions and precursors to conditions that mammography can't such as inflammation, estrogen dominance, and lymphatic congestion allowing for preventative steps to be taken.
Thermograms are also not limited to the 'compression area' like a mammogram. In fact, thermograms can be used to image the entire body, and part of a regular breast screening includes under the arms and the upper back.
Normal
Good thermal symmetry with no suspicious vascular patterns or significant thermal findings.
Fibrocystic Changes
The very significant vascular activity in the left breast justified clinical correlation and close monitoring which returned an opinion of fibrocystic changes taking place. These changes can be monitored thermographically at regular intervals until a stable baseline is established and is reliable enough for annual comparison.
Early Stage Malignant Tumor
This is the specific area of a small DCIS. We can see the vascular feed and the discreet area of hypothermia that is displacing the surrounding hyperthermia.
Breast thermograms are excellent for showing inflammation, lymphatic congestion and estrogen dominance, all precursors to disease allowing for early prevention, as well as inflammatory breast disease, fibrocystic and cystic breast, physiological changes associated with the early development of tumors, and a number of other conditions. However, while the evaluation of thermal patterns allows for detection of these conditions it can also prohibit finding other conditions such as a well established tumor. Imagine in a well established tumor it is such that it is not necessarily growing, not necessarily changing any longer; the thermal imaging might not be able to detect this due to lack of thermal activity.
Another drawback to thermography is that while concerning vascular activity might be identified it sometimes will not provide enough information to know more than that additional testing is needed. This is a problem with mammograms and other tests as well in that what is seen often requires additional testing and/or a biopsy, but with a thermogram being unable to identify structure a mammogram or ultrasound is always needed to clarify the thermographic readings. A test of structure (mammograms, ultrasounds, MRI's) should accompany a test of physiology (thermograms) and visa versa, which makes thermography an excellent tool alongside a test of structure.
3D Mammograms
3D mammography, also known as tomosynthesis or 3D breast imaging, is an advanced technology in the fight against breast cancer that allows doctors to examine your breast tissue one layer at a time. The 3D breast imaging system uses high-powered computing to convert digital breast images into a stack of very thin layers or “slices” for your radiologist to review.
A good analogy for a 3D mammogram is thinking of pages in a book. If you look down at the cover, you cannot see all of the pages – but when you open it up, you can go through the entire book page-by-page to see everything between the covers. 3D mammograms were designed with the same concept in mind.
In this regard, 3D mammograms are far superior to 2D mammograms, but they come with the same drawbacks and then some. First, the duration of the procedure is longer meaning longer exposure to radiation and compression and second, 3D mammograms are often done after having had the 2D mammogram meaning simply that much more radiation and compression.
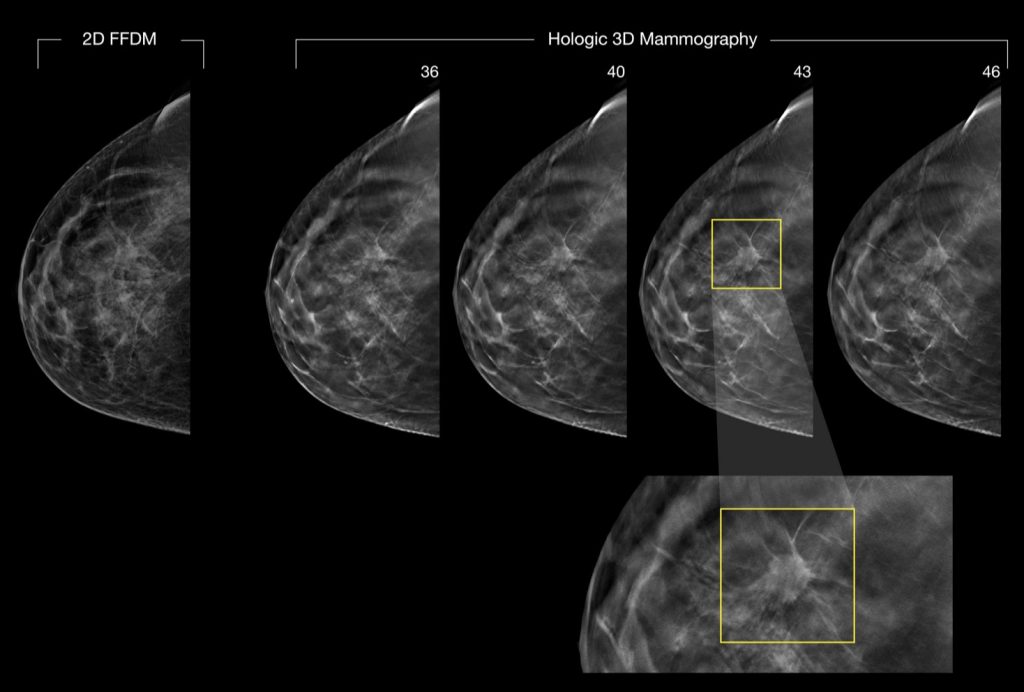
A malignancy easily missed with conventional 2D mammography was clearly seen with 3D mammography (5).
Ultrasound
Ultrasound imaging of the breast uses sound waves to produce pictures of the internal structures of the breast. It is primarily used to help diagnose breast lumps or other abnormalities your doctor may have found during a physical exam, mammogram, thermogram, or breast MRI. Ultrasound is safe, non invasive and does not use radiation.
Breast ultrasound is not usually done to screen for breast cancer. This is because it may miss some early signs of cancer. An example of early signs that may not show up on ultrasound are tiny calcium deposits called microcalcifications. (6)
Benefits
- Most ultrasound scanning is noninvasive (no needles or injections).
- Occasionally, an ultrasound exam may be temporarily uncomfortable, but it should not be painful.
- Ultrasound is widely available, easy-to-use and less expensive than most other imaging methods.
- Ultrasound imaging is extremely safe and does not use radiation.
- Ultrasound scanning gives a clear picture of soft tissues that do not show up well on x-ray images.
- Ultrasound provides real-time imaging, making it a good tool for guiding minimally invasive procedures such as needle biopsies and fluid aspiration.
- Ultrasound imaging can help detect lesions in women with dense breasts.
- Ultrasound may help detect and classify a breast lesion that cannot be interpreted adequately through mammography alone.
- Using ultrasound, physicians are able to determine that many areas of clinical concern are due to normal tissue (such as fat lobules) or benign cysts. For most women 30 years of age and older, a mammogram will be used together with ultrasound. For women under age 30, ultrasound alone is often sufficient to determine whether an area of concern needs a biopsy or not.
Risks
- Standard diagnostic ultrasound has no known harmful effects on humans.
- Interpretation of a breast ultrasound examination may lead to additional procedures such as follow-up ultrasound and/or aspiration or biopsy. Many of the areas thought to be of concern turn out to be non-cancerous (false positives). (7)
- Breast ultrasound is subject to the skill of the sonographer. Unlike a mammogram or thermogram that takes a complete image, a sonographer's error can result in a potential finding being missed.
MRI
Magnetic resonance imaging (MRI) of the breast — or breast MRI — is a test used to detect breast cancer and other abnormalities in the breast.
Using a powerful magnetic field and radio waves a breast MRI captures multiple images of your breast. Breast MRI images are combined, using a computer, to create detailed pictures.
A breast MRI usually is performed after you have a biopsy that's positive for cancer and your doctor needs more information about the extent of the disease. For some people, a breast MRI may be used with mammograms as a screening tool for detecting breast cancer. That group of people includes women with a high risk of breast cancer, who have a very strong family history of breast cancer or carry a hereditary breast cancer gene mutation.
As seen to the right a breast MRI has detected an advanced cancer in the left breast.
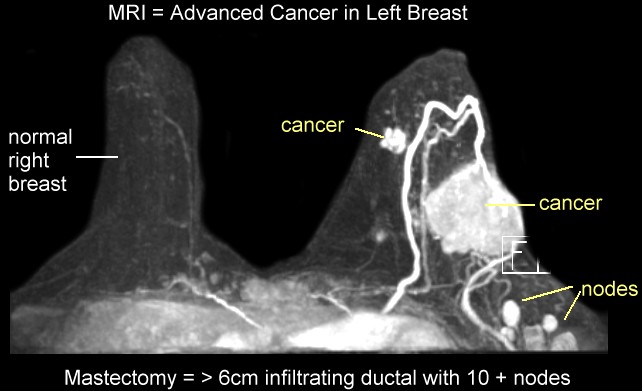
A breast MRI is a safe procedure that doesn't expose you to radiation. But as with other tests, a breast MRI has risks, such as reaction to the contrast dye used.
Breast MRI involves injection of a dye to make the images easier to interpret. This dye can cause allergic reactions and can cause serious complications for people with kidney problems. (8) This dye, gadolinium, can result in life-threatening toxicity. A 2016 study found common reactions included headaches, bone and nerve paid, and skin thickening presumed to be related to gadolinium toxicity. (9)
Summary
We want to strongly encourage that you discuss with your doctor what method of screening(s) is best for you. It is our belief and the medical science supports it that no one method suffices on its own; you need to weigh the pros and cons of all available methods and choose a 'package' that best suits your needs.
Remember that all tests have the potential for false-positives and false-negatives and every test has something it cannot or usually cannot see--they are limited to their specific scope--but some tests come with greater risks than others and should be considered carefully about how they may negatively impact your health.
Sources:
(1) https://www.fda.gov/consumers/consumer-updates/breast-cancer-screening-thermogram-no-substitute-mammogram
(2) http://www.preventcancer.com/patients/mammography/dangers.html
(3) https://www.breastcancer.org/research-news/device-could-reduce-mammogram-pain
(4) https://articles.mercola.com/sites/articles/archive/2012/03/03/experts-say-avoid-mammograms.aspx
(5) https://www.puremammo.com/mammography/advantages-3d-mammography/
(6) https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/breast-ultrasound
(7) https://www.radiologyinfo.org/en/info.cfm?pg=breastus#benefits-risks
(8) https://www.mayoclinic.org/tests-procedures/breast-mri/about/pac-20384809
(9) https://www.drugwatch.com/gadolinium/side-effects/