What is Abdominal Thermography?
Abdominal thermography is a specialized form of thermal imaging that focuses specifically on the abdominal region and the surrounding structures, including the lower back, pelvic area, and digestive organs. Using medical-grade infrared technology, this imaging method measures subtle temperature variations across the skin’s surface. These variations are not random—they often reflect underlying physiological or pathological processes, such as increased blood flow, inflammation, organ stress, muscular imbalance, lymphatic congestion, or early signs of dysfunction. Because the abdomen houses multiple vital organs and systems, thermal changes in this region can offer valuable insights into overall health.
Thermal imaging works by detecting infrared radiation naturally emitted by the body. When a thermal camera captures this information, it creates a visual map of temperature distribution. Areas that are unusually warm may indicate inflammation, irritation, infection, or hyperactivity of certain tissues or organs. Conversely, areas that appear cooler may reflect reduced circulation, nerve impairment, or structural restriction. These thermal patterns help practitioners identify where physiological changes may be occurring long before they produce overt symptoms.
One of the primary advantages of abdominal thermography is its ability to highlight functional changes rather than structural abnormalities alone. Traditional imaging tools—such as CT scans, MRIs, or ultrasounds—are excellent at revealing anatomical issues, but they often cannot detect early-stage physiological irregularities. Thermography fills this gap by focusing on how the body is behaving in real time. This makes it especially useful for monitoring chronic conditions, identifying patterns related to inflammation, or providing supportive information for patients experiencing digestive discomfort, hormonal imbalance, unexplained abdominal pain, or musculoskeletal issues in the lower back and pelvis.
Abdominal thermography is completely non-invasive and requires no radiation, no contrast dye, and no physical contact. The imaging process is simple: the patient stands in front of a thermal camera in a temperature-controlled room while several images are taken from different angles. The session is quick, comfortable, and suitable for individuals seeking a safe, repeatable method of monitoring physiological changes over time.
Once captured, the images are analyzed by trained thermographers who look for temperature asymmetries, vascular patterns, and regions that deviate from typical thermal behavior. These findings may help guide further evaluation, encourage preventive care, or provide additional information to healthcare providers who are managing digestive, metabolic, hormonal, or musculoskeletal conditions.
By offering a unique view of physiological function, abdominal thermography serves as a valuable tool for early detection, ongoing monitoring, and comprehensive wellness assessment.
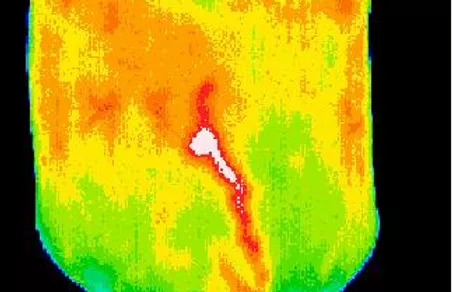
An abdominal thermography series can reveal a wide range of physiological concerns, including digestive disorders, organ dysfunction, colon irritation or inflammation, lower-back pain patterns, disc disease, muscular imbalance, and circulatory or lymphatic congestion. These thermal indicators provide valuable insight into how the abdominal and lower spinal regions are functioning beneath the surface.
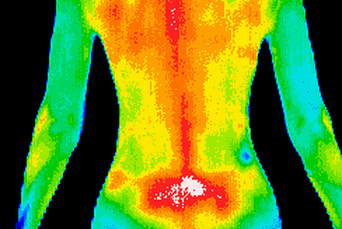
“Visualizing” lower back pain is extremely valuable because pain often radiates and is felt in areas far from its true origin. Thermography helps pinpoint the underlying source by identifying temperature changes, inflammation, and circulation patterns, giving providers a clearer understanding of where the pain begins and how it may be spreading.
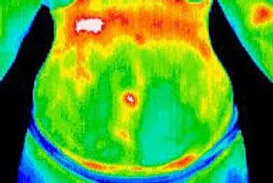
This thermogram shows the abdomen of a patient diagnosed with hepatitis. The previously closed hepatic blood vessel, which normally seals after birth, has reopened and is now visible extending from the liver to the umbilicus. This abnormal vascular activity highlights inflammation and altered liver function detected through thermal imaging.
Benefits of Abdominal Thermography
- Non-invasive & radiation-free: Unlike CT scans, X-rays or some other imaging modalities, thermography merely senses the heat radiation emitted by the body—no ionizing radiation involved.
- Quick & patient-friendly: A thermographic scan typically involves standing or lying in a prepared state, and capturing thermal images. It’s painless, doesn't require contrast agents, needles or incisions.
- Can detect subtle changes early: Because the method is sensitive to surface temperature changes, it may pick up early vascular/perfusion changes or inflammation before structural changes become obvious.
- Provides a visual map: The thermogram shows a thermal “map” of the region. For practitioners trained in interpretation, this can offer insight into patterns of dysfunction — not just isolated numbers.
- Complementary tool: It can serve as an adjunct to other diagnostic approaches (clinical exam, lab tests, imaging) rather than wholly replacing them. For example, if someone has vague abdominal/back pain, thermography may add data to guide further testing.
- Ideal for ongoing monitoring: Because it is safe for repeated use, thermography is well suited for tracking chronic conditions, post-surgical healing, or long-term inflammation without exposing patients to repeated radiation.
- Helps identify functional issues: While structural imaging focuses on anatomy, thermography highlights functional or physiologic problems—such as circulation irregularities, lymphatic congestion, or organ stress—that may not appear on traditional scans.
- Useful for complex or unexplained symptoms: For patients with diffuse abdominal discomfort, intermittent pain, or symptoms that don’t align with structural findings, thermography can reveal patterns that point providers toward the true underlying cause.
Why the Abdomen?
- The abdomen houses many organs (liver, stomach, intestines, pancreas), the abdominal wall, and is connected to the lower back via structural anatomy (vertebrae, discs, nerves). Thus many dysfunctions may manifest as changes in heat distribution.
- For example, if a disc disease in the lower back is causing referred pain or sympathetic changes, the overlying abdominal region may show subtle thermal anomalies.
- The Thermography Advantage website suggests: “Pain often radiates and is felt elsewhere from where it actually originates. Thermography can help identify the source of pain.”
- Because the abdomen is a crossroads of digestive, lymphatic, endocrine, and musculoskeletal systems, thermal changes here can serve as early indicators of multi-system dysfunction before symptoms become severe.
- The abdominal region contains major blood vessels, including branches of the aorta and iliac arteries; vascular inflammation or circulatory issues may present as temperature asymmetry long before structural changes develop.
- The gut plays a major role in immune response and inflammation. Conditions such as IBS, gastritis, liver stress, or visceral inflammation often create recognizable thermal signatures that help guide further evaluation or targeted care.
What to Expect During an Abdominal Thermography Study
Here’s a practical overview of how a typical abdominal thermography session might be conducted:
-
Preparation
-
The patient may be asked to avoid heavy exercise, caffeine, nicotine, hot or cold packs, or anything that significantly stimulates or suppresses circulation for several hours before the scan. These precautions help ensure that the abdominal thermal patterns reflect true physiological activity rather than temporary external influences.
-
The ambient temperature in the imaging room is carefully stabilized to eliminate external thermal influences. Maintaining a controlled environment ensures that any heat patterns detected during the scan come from the patient’s physiology—not from drafts, temperature shifts, or environmental factors that could distort the accuracy of the results.
-
-
-
Imaging
-
-
The technician ensures consistent positioning and posture, maintains proper focus, and verifies accurate emissivity calibration of the camera. A standardized distance between the patient and imaging device is carefully maintained to guarantee uniform image quality and reliable thermal data across all captured abdominal views.
-
-
Image Processing & Interpretation
-
The captured thermogram displays a range of thermal gradients, typically shown in color-coded patterns that transition from cooler to warmer areas. These variations highlight differences in circulation, inflammation, and surface temperature, allowing practitioners to visually interpret physiologic activity across the abdominal region with greater clarity.
- A trained clinician or thermographer evaluates the images by assessing left-to-right symmetry, identifying hot and cold spots, and examining how heat spreads across the region. These thermal patterns help reveal inflammation, circulation issues, nerve involvement, or other physiologic changes that may indicate underlying abdominal or lower-back dysfunction.
-
For example, the Thermography Advantage site highlights a case in which an enlarged, reopened hepatic blood vessel appeared as an abnormal thermal pattern in a patient with hepatitis. This distinct temperature signature helped identify underlying liver inflammation not immediately visible through traditional structural imaging.
-
-
Report & Follow-Up
- The report typically documents any abnormal thermal patterns and explains their potential significance. It may correlate these findings with the patient’s symptoms—such as abdominal pain, digestive disturbances, or back pain—and recommend appropriate next steps, including lab work, additional imaging, or referral to a specialist if needed.
-
Because thermography provides a single snapshot of physiologic activity at one point in time, clinicians may recommend follow-up scans. Repeat imaging helps monitor whether thermal patterns improve with treatment, remain stable, or show signs of worsening, offering valuable insight into progression or recovery.
Frequently Asked Questions
- Can lifestyle factors such as diet, exercise or stress affect the thermal patterns seen in an abdominal thermography scan?
- If an abnormal thermal pattern shows up in the abdomen, what are typical next steps for follow-up or assessment?
- Are there particular preparation guidelines or conditions a patient should follow before an abdominal thermography scan to ensure accurate and consistent results?
Q1: Can lifestyle factors such as diet, exercise or stress affect the thermal patterns seen in an abdominal thermography scan?
Answer: Absolutely. The heat emissions captured by infrared imaging reflect underlying physiology — including blood flow, inflammation, nerve activity, and metabolic processes. For example, a heavy processed‐food diet or frequent alcohol use may trigger low-grade inflammation in the gut or liver, which could show up as warmer thermal zones. Similarly, intense or irregular workouts might lead to muscular strain or vascular changes in the abdominal region that influence a scan. Chronic stress can alter nerve tone and circulation, also influencing temperature patterns. The bottom line: While thermography detects functional changes (not anatomical ones), these functional changes are often modifiable through lifestyle. Using the scan as a “before and after” marker of lifestyle shifts (improved diet, more consistent sleep, better stress management) can enhance its practical value.
Q2: If an abnormal thermal pattern shows up in the abdomen, what are typical next steps for follow-up or assessment?
Answer: When a thermography scan reveals an unusual thermal asymmetry or “hot” or “cold” spot in the abdomen, it doesn’t immediately point to a specific organ or diagnosis — but it does serve as a functional red flag. The next steps usually include:
-
Reviewing the scan with a qualified thermography clinician who understands what the pattern might indicate (e.g., increased inflammation, altered nerve or vascular activity).
-
Correlating the scan findings with the patient’s history, symptoms (e.g., pain, bloating, digestive changes), labs, and any prior imaging.
-
Depending on the findings, ordering more targeted anatomical imaging (ultrasound, MRI, CT), or interventional tests (e.g., blood work for liver/pancreas, GI endoscopy) to rule in/out structural abnormalities.
-
Implementing lifestyle or therapeutic interventions (anti-inflammatory diet, exercise adjustments, injury/strain investigation, stress reduction) and repeating the scan in a defined interval (e.g., 3-6 months) to monitor change.
Thus, thermography in the abdomen functions mostly as an early alert system — not a stand-alone diagnostic tool — and is most useful when integrated with other clinical assessments.
Q3: Are there particular preparation guidelines or conditions a patient should follow before an abdominal thermography scan to ensure accurate and consistent results?
Answer: Yes — because thermography detects subtle thermal differences, it’s highly sensitive to external and internal influencing factors. For best accuracy and consistency in abdominal scans, patients are typically advised to:
-
Avoid vigorous exercise for at least 12–24 hours before the scan (exercise can alter blood flow/heat in abdominal muscles or organs).
-
Fast for a few hours (often 2–4 hours) prior to the scan to reduce recent digestive‐activity heat variation.
-
Refrain from drinking hot or cold beverages just before the test (extreme temperature exposures can transiently alter abdominal skin/organ heat).
-
Avoid applying lotions, oils or topicals on the abdomen within 24 hours (these can insulate or alter skin emissivity).
-
Ensure the scanning room is temperature-controlled and acclimate for a set period (e.g., 10-15 minutes) without tight clothing or obstructive accessories.
-
Maintain consistent conditions from scan to scan if follow-up imaging is planned (same time of day, same preparations) so that comparisons are meaningful.
Following these protocols helps ensure the scan captures internal functional changes — not artifacts or external influences — making the results far more reliable for tracking over time.