Unlocking the Potential of Thermographic Evaluation: What Conditions Can Thermal Imaging Help Detect?
Thermographic evaluation — a non-invasive imaging technique that measures subtle temperature variations across the body’s surface — is increasingly recognized for its supportive role in modern diagnostics. By capturing thermal patterns related to circulation, inflammation, neural activity, and autonomic function, thermography provides physiologic information that may not appear on structural scans such as X-ray, ultrasound, or MRI. At Thermography Advantage, we use this advanced technology to uncover early indicators and temperature-based abnormalities that may relate to a broad range of structural, vascular, neural, musculoskeletal, and skin-related conditions.
Because thermography evaluates function rather than anatomy, it often highlights physiologic changes before structural damage is visible. This makes it a valuable complementary tool for individuals experiencing unexplained symptoms, complex pain patterns, recurrent injuries, or concerns that have not been fully explained by other tests. By observing how different areas of the body respond thermally, clinicians gain insights into dysfunctions such as inflammation, nerve irritation, circulatory irregularities, biomechanical stress, lymphatic congestion, and autonomic nervous system imbalance.
It’s important to view thermography as one piece of a larger clinical picture rather than a standalone diagnostic method. While it excels at detecting physiologic anomalies — such as temperature asymmetry, thermal inflammation markers, and sympathetic responses — these findings guide further evaluation rather than replace traditional medical testing. When interpreted alongside a patient’s symptoms, history, physical exam, and additional imaging, thermography helps build a more complete and accurate understanding of what may be occurring beneath the surface.
At Thermography Advantage, our goal is to provide meaningful, actionable thermal insights that support early detection, improve monitoring, and empower both patients and providers in making informed decisions about health and wellness.
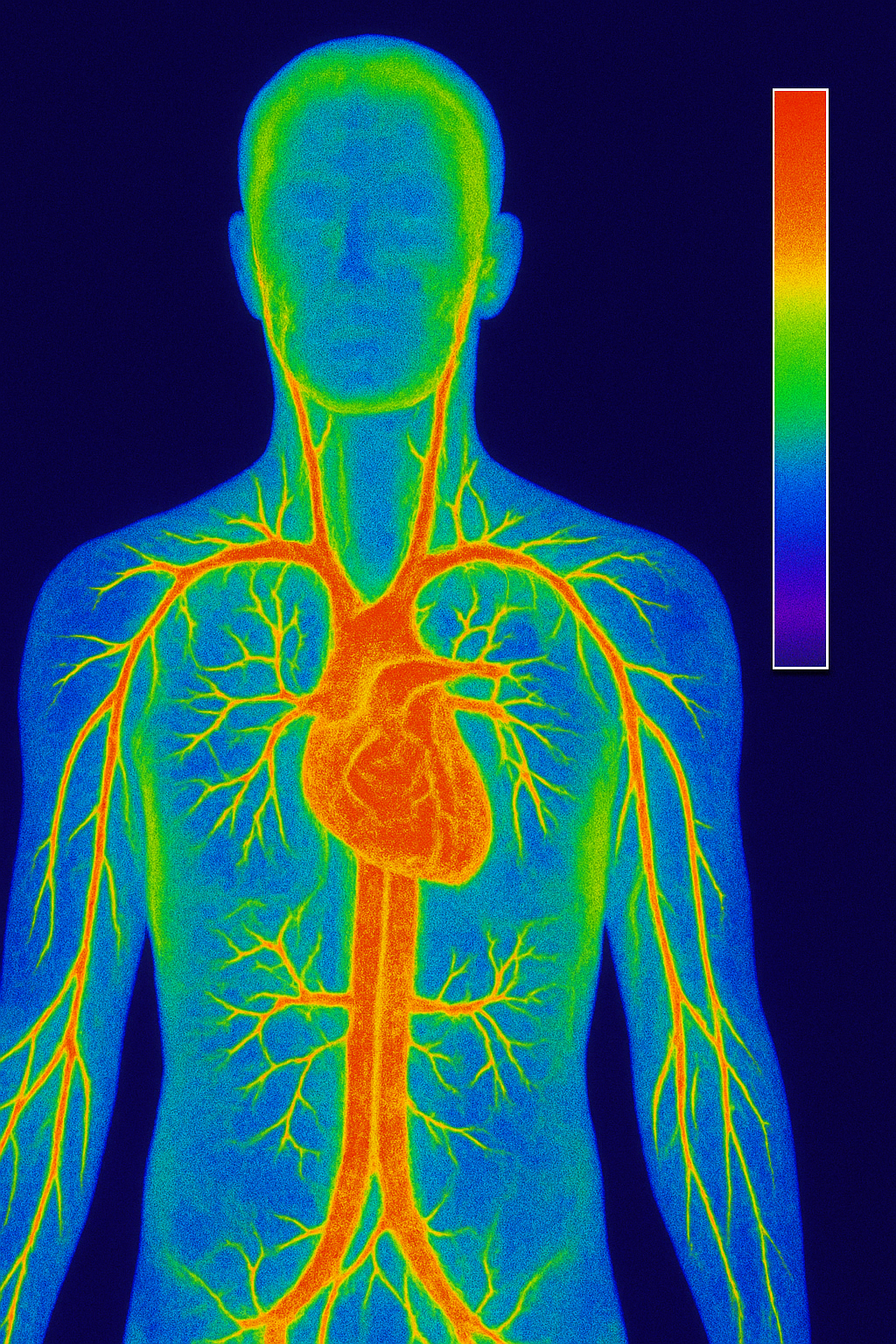
Vascular & Circulatory Indicators
Thermography is particularly valuable when evaluating circulation, because changes in blood flow often create distinct thermal patterns long before structural damage becomes visible on traditional imaging. When veins or arteries are functioning abnormally, the body responds with alterations in heat distribution—either warmer areas caused by inflammation and increased metabolic activity or cooler regions resulting from reduced perfusion or vascular constriction. These shifts can be subtle, but thermal imaging is sensitive enough to detect them early.
By capturing these temperature variations on the skin’s surface, thermography provides important physiologic clues about emerging vascular concerns. Irregular thermal patterns may suggest compromised venous return, arterial insufficiency, developing inflammation, or localized circulatory stress. While this information does not diagnose specific vascular diseases on its own, it can alert clinicians to areas that warrant closer examination through additional testing.
Used as part of a comprehensive evaluation, thermography enhances clinical awareness, supports early intervention, and helps track changes in vascular health over time.
Some vascular-related conditions thermography may help detect include:
-
Arteriosclerosis and superficial vascular disease – When blood vessels become narrowed or hardened, circulation slows and affected regions may appear cooler or show uneven temperature patterns. These thermal irregularities can provide early clues about reduced perfusion or developing blockages.
-
Internal or external carotid insufficiency – Because the carotid arteries supply blood to the brain and surrounding tissues, disruptions or narrowing can cause temperature asymmetry in the head, neck, and facial regions. Thermography may highlight these variations, prompting further vascular evaluation.
-
Raynaud’s phenomenon and other vasospastic conditions – Episodic constriction of blood vessels in the extremities (such as fingers, toes, ears, or nose) can create dramatic thermal shifts. During or after an episode, thermography may capture patterns of reduced warmth, delayed reperfusion, or asymmetrical temperature recovery—useful for monitoring severity or treatment response.
-
General circulatory insufficiency or altered heat dissipation – Even without a specific diagnosis, thermography can reveal areas where blood flow is impaired, where inflammation is concentrated, or where autonomic regulation of vascular tone is disrupted.
By visualizing how blood moves—or fails to move—through the body, thermography provides meaningful functional insight that complements traditional anatomical imaging. Instead of viewing structure alone, clinicians can observe temperature patterns that reflect real-time circulatory performance. These thermal cues may reveal early vascular changes, areas of impaired perfusion, or regions experiencing inflammation or autonomic imbalance. When combined with a patient’s symptoms and medical history, thermography becomes an important adjunctive tool for tracking circulation-related concerns, monitoring progression, and determining whether additional vascular testing is necessary. This added layer of information supports more precise clinical decision-making and earlier intervention when needed.
Neural & Nerve Injury Issues
Because nerves regulate vascular response (among other mechanisms), thermographic readings can reveal areas of abnormal nerve-vascular interplay. Possible indications include:
-
Neuropathy, nerve stretch injury, nerve entrapment or impingement
-
Nerve root irritation, peripheral nerve injury, and axon disease
-
Neuralgia, neuritis, or conditions affecting lower motor neurons or plexuses
Musculoskeletal & Soft Tissue Conditions
Thermography is also widely used to assess temperature patterns associated with musculoskeletal stress, injury, or inflammation. When muscles, tendons, ligaments, or joints become irritated or overworked, they often produce subtle thermal changes that appear as localized hot or cold areas on a thermographic scan. These patterns can help identify regions of strain, early inflammatory responses, or biomechanical imbalances that may not yet be apparent through structural imaging. By monitoring these thermal shifts over time, clinicians can track healing progress, evaluate treatment effectiveness, and detect lingering dysfunction that could increase the risk of re-injury. This makes thermography a valuable tool in musculoskeletal evaluation and recovery planning. These may include:
-
Tendonitis, bursitis, ligament tears, muscle tears, sprain/strain injuries
-
Soft tissue injury, myofascial irritation or spasm, trigger points
-
Spinal-related conditions like herniated or ruptured discs, facet syndromes, and whiplash injuries
Spinal, Disc & Biomechanics-Related Evaluations
Because structural misalignments, disc issues, or impaired biomechanics often trigger altered nerve function, inflammation, or changes in vascular response, thermography can play a meaningful role in evaluating these concerns. Abnormal temperature patterns along the spine or surrounding musculature may indicate irritated nerves, dysfunctional movement patterns, compensatory muscle activity, or areas experiencing excessive mechanical stress. These thermal cues can help clinicians identify regions of concern earlier, even when structural imaging has not yet revealed significant changes. By comparing patterns over time, thermography supports monitoring of disc-related symptoms, postural strain, and responses to chiropractic, physical therapy, or rehabilitative treatments—helping guide a more targeted and effective care plan. Thermography can assist in assessing:
-
Disc disease, disc syndromes such as herniated nucleus pulposus
-
Biomechanical impropriety, altered ambulatory or biokinetic patterns
-
Conditions like thoracic outlet syndrome, cord injury, brachial plexus injury
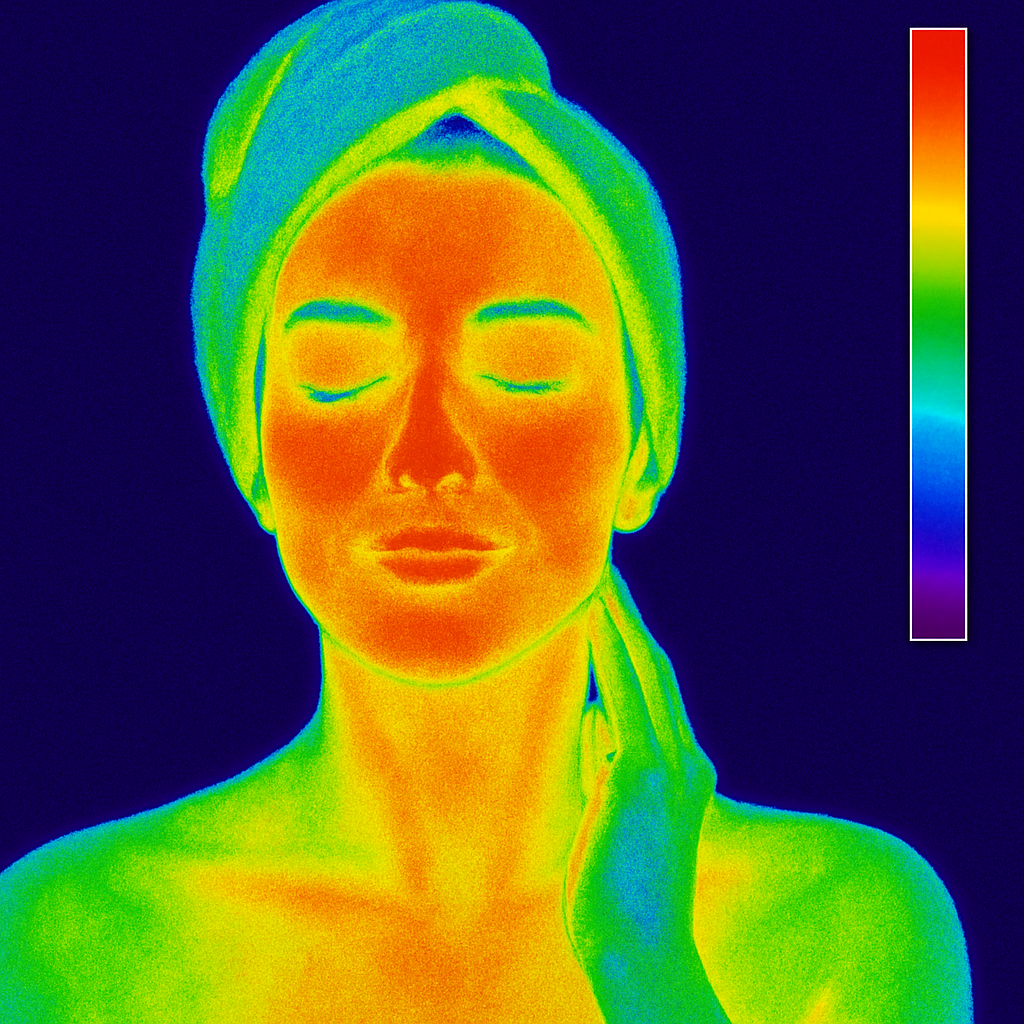
Skin & Superficial Conditions
Thermography is especially effective when evaluating the body’s surface, where even small variations in temperature can signal meaningful physiological changes. Because the skin responds rapidly to shifts in inflammation, irritation, blood flow, and autonomic activity, thermal imaging can reveal subtle patterns that might otherwise go unnoticed during a routine exam. These temperature variations—whether warmer areas indicating increased metabolic activity or cooler zones suggesting reduced circulation—provide valuable clues about how different regions of the body are functioning beneath the surface.
This makes thermography particularly useful for identifying early abnormalities, tracking evolving symptoms, or monitoring how specific conditions respond to treatment over time. Even when structural imaging such as X-ray, ultrasound, or MRI appears normal, surface temperature changes may offer additional context that helps clinicians pinpoint dysfunction or decide whether further evaluation is needed. By capturing these physiologic signals, thermography adds an important layer of insight to the diagnostic and monitoring process, supporting more informed and proactive patient care.
These patterns can help identify:
-
Skin abnormalities, including temperature variations associated with melanomas, basal cell carcinoma, or squamous cell changes. While thermography is not a standalone diagnostic tool, it can highlight areas that may need further dermatological evaluation.
-
Infectious conditions that alter thermal behavior in the skin, such as shingles, cellulitis, or certain bacterial or neurologic infections that create distinctive heat signatures.
-
Inflammatory and superficial vascular responses, where localized hotspots or cooler regions may correspond to irritation, trauma, or altered blood flow near the surface.
By capturing these subtle temperature dynamics, thermography adds an additional layer of insight into skin and superficial tissue health, helping guide clinicians toward areas that may warrant closer attention.
Other Areas of Use
The list of possible detectable conditions is extensive, and thermography is used in many less-common clinical contexts as well. Because it highlights physiologic changes rather than structural abnormalities, thermal imaging can reveal early indicators across a wide range of concerns. Beyond the more familiar vascular, musculoskeletal, and neurological applications, thermography may also assist in evaluating autoimmune activity, chronic pain patterns, dental or sinus inflammation, post-surgical healing, and temperature changes linked to hormonal imbalance or lymphatic congestion. These additional uses make it a versatile adjunctive tool, offering clinicians valuable insight in cases where traditional imaging may provide limited information.
-
Stroke screening, referred pain syndrome, somatic or somatization disorders
-
Headache evaluations, TMJ dysfunction (temporomandibular joint), trigeminal neuralgia
-
Nutritional disease effects (for example diabetes, alcoholism) which affect vascular or nerve health
Important Considerations
-
Adjunct, not replacement: Thermography provides valuable clues by capturing thermal patterns, but it’s not intended to replace definitive diagnostic testing (such as MRI, ultrasound, or laboratory analyses).
-
Interpretation matters: Temperature variations may arise from many causes — vascular changes, nerve dysfunction, inflammation, biomechanics, or surface factors (like ambient temperature or skin condition). It’s critical to interpret thermographic findings within the broader clinical context.
-
Tailored to your situation: Because every body is unique, and because thermography is sensitive to many variables, we encourage a consultative approach. If you have a condition not listed above, feel free to contact us — we can discuss whether thermal imaging may be helpful in your specific scenario.
Final Thoughts
The power of thermographic evaluation lies in its ability to non-invasively visualize thermal changes that often accompany underlying physiological or structural dysfunction. Instead of focusing on anatomy alone, thermography captures the body’s functional responses — subtle shifts in heat that can reflect inflammation, vascular changes, nerve irritation, autonomic imbalance, or biomechanical stress. These temperature patterns provide a layer of insight that many traditional imaging methods cannot detect, especially in the earliest stages of a developing condition.
Because the skin is highly responsive to changes in circulation, nerve activity, and tissue stress, thermal mapping becomes a meaningful window into how the body is functioning beneath the surface. Warmer or cooler regions may indicate irritation, compromised blood flow, overuse, or compensatory movement patterns. Even when X-rays, MRIs, or ultrasounds appear normal, these thermal signals can help direct attention to areas that may benefit from closer evaluation or early intervention.
This makes thermography a valuable adjunctive tool for a wide variety of clinical contexts. Individuals dealing with nerve-related symptoms, chronic or unexplained pain, circulatory concerns, repetitive strain, or musculoskeletal injuries may gain additional clarity from the physiologic perspective thermography provides. The technology can help identify patterns that support earlier detection, illuminate issues that are difficult to see structurally, and assist in determining whether symptoms are progressing, improving, or shifting over time.
For healthcare providers, thermography adds another dimension to the diagnostic and monitoring process. Serial imaging allows clinicians to compare thermal patterns across visits, offering objective documentation of change. This is especially helpful when managing chronic pain, tracking inflammation, evaluating treatment effectiveness, or screening areas of concern that warrant follow-up with more targeted diagnostic tests.
When used thoughtfully and in conjunction with standard evaluations, thermography enhances the overall quality of clinical decision-making. It is not meant to replace other diagnostic methods, but rather to complement them — offering extra context, physiologic detail, and early indicators that might otherwise be missed. For patients and providers alike, this added layer of information can lead to more informed choices, earlier interventions, and a clearer understanding of what may be occurring beneath the surface of the skin
If you’re curious whether thermography is right for you, reach out today and let’s explore how it may support your health journey.
Frequently Asked Questions
- If I’ve already had a standard imaging test (like MRI or ultrasound), why should I consider getting a thermography scan at Thermography Advantage?
- Are there any conditions or situations where thermography might not be appropriate or enough by itself for diagnosis?
- If I get a thermography scan and the results show something abnormal (for example increased temperature asymmetry), what are the next steps?
Q1: If I’ve already had a standard imaging test (like MRI or ultrasound), why should I consider getting a thermography scan at Thermography Advantage?
A: While MRI, ultrasound and similar tests focus primarily on structure (e.g., tissue anatomy, masses, lesions), a thermography scan focuses on physiology — the way your body is functioning, especially in terms of heat & blood-flow patterns. This means thermography can detect subtle changes (like inflammation, nerve irritation, altered vascular flow) sometimes before structural changes become visible. If you’re looking for a more proactive snapshot of physiological stress, thermography can add value in addition to structural imaging.
Q2: Are there any conditions or situations where thermography might not be appropriate or enough by itself for diagnosis?
A: Yes. It’s important to know that thermography is a valuable tool but not a standalone solution in every scenario. For example, when it comes to breast cancer screening, the Food and Drug Administration (FDA) states that thermography has not been proven to be effective as a standalone method for early breast-cancer detection. The technique detects surface/infrared heat changes — but it doesn’t replace structural imaging like mammography when structural abnormalities are present. So, if your clinician suspects a structural lesion, standard imaging and clinical evaluation are still essential.
Q3: If I get a thermography scan and the results show something abnormal (for example increased temperature asymmetry), what are the next steps?
A: Great question! An abnormal thermal finding indicates that something is going on physiologically (for instance inflammation, nerve irritation, vascular change). The next steps typically include:
-
A clinical evaluation to correlate the thermal findings with symptoms, history and physical exam.
-
Possibly ordering more specific structural imaging or laboratory work to localize and identify the exact cause.
-
A consult with your healthcare provider (or a specialist) to interpret how the thermography results fit into your overall health picture.
-
Developing a follow-up plan: monitoring with repeated thermography, intervening (lifestyle, therapy, etc.), or treating an identified condition. Because thermography is about early detection of physiological shifts, the goal is often prevention or earlier intervention rather than waiting.