2D Mammograms, Thermograms, 3D Mammograms, Ultrasounds, MRI's--which is the right choice?
With so many breast-screening options available today, it’s completely understandable to feel unsure about which test is right for you. Each modality—2D mammograms, 3D mammograms, thermography, ultrasounds, and MRI scans—offers its own strengths, limitations, and role in the bigger picture of breast health. None of these tests is a perfect, stand-alone solution. Instead, each provides a different “piece of the puzzle,” revealing information from a unique angle. When combined thoughtfully, these pieces create a more complete, accurate, and empowering understanding of your breast health.
The purpose of this article is to help you clearly understand what each imaging method can and cannot do. By breaking down the advantages and limitations of every option, you’ll be better equipped to make truly informed decisions—decisions that are based on knowledge, comfort, and collaboration with your healthcare provider rather than uncertainty or fear.
While we are thermography providers, we want to be completely transparent: thermography is not the only screening tool you should rely on. And this article is not intended to convince you to choose thermography over anything else. Every woman is unique. Breast density varies, medical history varies, risk levels vary, and personal preferences vary. Because of this, no single imaging method will meet the needs of every woman in every situation.
Thermography absolutely has value—particularly in identifying early physiologic changes long before structural changes occur. Its ability to capture heat, inflammation, and vascular patterns can be incredibly helpful for proactive monitoring. But just like mammography, ultrasound, and MRI, thermography also has its limitations. It does not replace structural imaging, nor does it serve as a sole diagnostic test. It is one tool in a much larger toolkit.
2D and 3D mammograms remain the standard structural imaging methods for identifying masses, calcifications, and other anatomical changes. Ultrasounds provide additional clarity, especially in dense breast tissue or in evaluating specific areas of concern. MRI is one of the most sensitive imaging options available, often used for high-risk patients or complex diagnostic questions. Each of these tests brings something important to the table, and understanding how they work together can dramatically improve your long-term breast-health strategy.
Our goal is simply to empower you. We want you to know what each test is capable of, how it complements the others, and when each may be appropriate. By understanding their roles—whether for early detection, structural evaluation, or physiological monitoring—you can confidently work with your medical provider to develop a customized screening plan that fits your body, your history, and your peace of mind.
The more informed you are, the better equipped you’ll be to make decisions that truly support your health. And when your screenings work together instead of competing with each other, you gain a stronger, clearer, and more complete picture of your breast health than ever before.
2D Mammograms
2D mammograms are the most widely recognized and commonly recommended method for breast screening. As the long-standing standard in breast imaging, they have been used for decades and continue to be heavily relied upon by physicians, clinics, and national health organizations. The FDA not only approves mammography as a primary screening tool but also requires that healthcare providers recommend a mammogram before suggesting many other imaging options. For this reason, mammograms are often referred to as “the gold standard” in breast screening.
A 2D mammogram works by compressing the breast tissue between two plates and taking X-ray images from the front and side. These images allow radiologists to see structural changes such as calcifications, masses, or distortions within the breast tissue. Because it focuses on anatomy rather than function, a mammogram’s strongest value lies in identifying physical abnormalities that have already formed. It has saved countless lives by detecting breast cancer early enough for successful treatment, which is why it remains so widely recommended.
However, like all imaging tools, 2D mammography has both strengths and limitations. Its biggest advantage is accessibility and familiarity; most medical centers offer mammograms, and radiologists are extensively trained to interpret them. It is particularly effective in detecting certain types of calcifications, which sometimes serve as the earliest structural signs of cancer.
On the other hand, 2D mammograms can be less effective for women with dense breast tissue. Density can obscure potential abnormalities, making it harder to distinguish between normal tissue and areas of concern. Dense breasts appear white on the X-ray—and so do many forms of cancer—resulting in reduced accuracy and occasional false negatives. This is why many states now require that women with dense breasts be informed about the limitations of mammography and their options for additional screening.
Mammograms also expose the breast to a small amount of radiation, which some women prefer to minimize. And while the compression involved is generally safe, it can be uncomfortable or even painful for certain individuals.
Despite these limitations, 2D mammography remains a valuable part of a comprehensive breast-screening strategy. It provides critical structural information that other tests—such as thermography, ultrasound, or MRI—cannot replace. Understanding both its capabilities and its shortcomings helps women make informed decisions and create a breast-health plan that incorporates the best tools for their unique needs.
Thermography
Breast thermography is a safe, non-invasive imaging method that identifies early physiologic changes in breast tissue—changes that may appear long before anything can be detected through a mammogram, ultrasound, or physical exam. Instead of looking for structural abnormalities, such as masses or calcifications, thermography evaluates function. It measures patterns of heat, inflammation, and vascular activity that reflect how the breast tissue is behaving in real time. These physiologic signals are often the earliest indicators that something in the breast may be changing.
By capturing detailed thermal images with medical-grade infrared cameras, thermography can reveal subtle variations in temperature and blood flow that correspond to hormonal imbalance, vascular development, lymphatic congestion, inflammation, or early indicators of potential disease. Because abnormal cells often create increased metabolic heat or require additional blood supply, thermography is uniquely positioned to identify these early physiological patterns.
One of the most appealing features of breast thermography is its total safety. There is no radiation exposure, no compression of the breast tissue, and no physical contact of any kind. The imaging session is fast, comfortable, and risk-free, making it an excellent choice for women seeking a gentler screening option or those who prefer to avoid repeated radiation exposure.
When thermography is combined with structural imaging—such as mammography, ultrasound, or MRI—it provides a fuller, more comprehensive understanding of breast health. Thermography does not replace these tests, but it adds an invaluable layer of early physiologic insight. This combination supports earlier detection, clearer monitoring over time, and a more proactive approach to long-term breast wellness.
Normal
Good thermal symmetry with no suspicious vascular patterns or significant thermal findings.
Fibrocystic Changes
The very significant vascular activity in the left breast justified clinical correlation and close monitoring which returned an opinion of fibrocystic changes taking place. These changes can be monitored thermographically at regular intervals until a stable baseline is established and is reliable enough for annual comparison.
Early Stage Malignant Tumor
This is the specific area of a small DCIS. We can see the vascular feed and the discreet area of hypothermia that is displacing the surrounding hyperthermia.
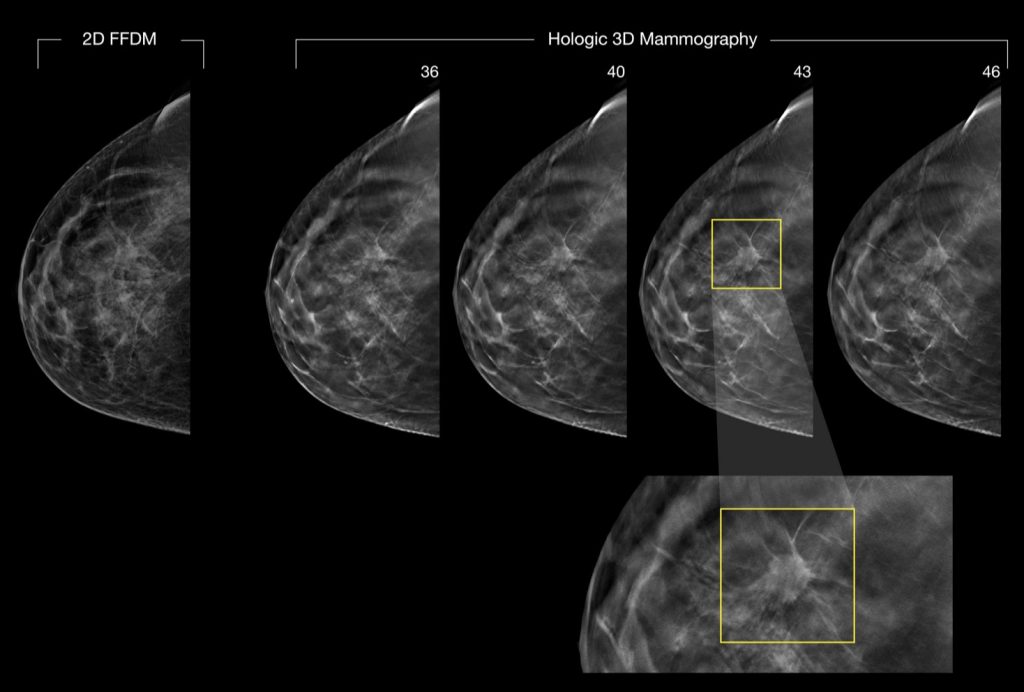
3D Mammograms
3D mammography, also called tomosynthesis or 3D breast imaging, is an advanced screening technology that has become increasingly common in the fight against breast cancer. Unlike traditional 2D mammography, which produces flat images of the breast, 3D mammography captures multiple images from different angles and reconstructs them into thin, layered “slices.” These slices allow radiologists to examine breast tissue one layer at a time, reducing the overlap of structures and making it easier to detect abnormalities that might otherwise be hidden.
A helpful way to visualize how a 3D mammogram works is to imagine a closed book. When you look only at the cover, you have no way of seeing the pages inside. A traditional 2D mammogram provides a similar single, flattened view. But when you open the book and flip through page by page, you’re able to examine every detail within. This page-by-page clarity is what 3D mammography brings to breast imaging: it reveals more information, reducing ambiguity and helping physicians better interpret complex breast tissue—especially in women with dense breasts.
Because of this layered imaging ability, 3D mammograms are considered superior to 2D mammograms in terms of structural visualization. They are better at identifying small masses, architectural distortion, and other early signs of breast cancer that might be obscured in a traditional 2D scan. Research supports improved detection rates and fewer false positives, which means fewer women are called back for unnecessary follow-up imaging.
However, even with these advantages, 3D mammography carries many of the same drawbacks as 2D mammography—and in some cases, additional considerations. The imaging process typically takes longer, which means prolonged compression of the breast and extended exposure to radiation. Although radiation levels remain within FDA-approved limits, some women prefer to minimize cumulative exposure, especially if they undergo yearly screenings or additional diagnostic imaging.
Another practical concern is that many facilities perform a 2D mammogram in combination with the 3D scan. While this approach provides both traditional and layered images for comparison, it also means even more compression and radiation during the same appointment. Not every patient feels comfortable with this increased exposure, particularly those who are seeking gentler or radiation-free screening options.
Despite these limitations, 3D mammography remains a valuable structural imaging tool. When paired with functional assessments like thermography or ultrasound, it contributes to a more complete, multi-dimensional understanding of breast health—allowing patients and providers to make better-informed decisions about ongoing monitoring, evaluation, and care.
Ultrasounds
Ultrasound imaging of the breast uses high-frequency sound waves to create detailed pictures of the internal structures of breast tissue. Unlike X-ray–based imaging, ultrasound does not use radiation, making it a safe and non-invasive option that can be performed as often as needed. It is painless, comfortable, and widely accessible, which is why healthcare providers frequently use it as a diagnostic tool when something unusual is detected during a physical exam, mammogram, thermogram, or breast MRI. Ultrasound is especially useful for clarifying the nature of a lump—helping determine whether it is solid, fluid-filled, or cystic.
While ultrasound is a valuable tool, it’s important to understand how it fits into breast-health screening. Breast ultrasound is typically not used as a primary screening test for breast cancer. This is because ultrasound, though excellent at distinguishing textures and fluid structures, may miss some of the earliest indicators of breast disease. For example, one of the most common early signs of breast cancer is the presence of tiny calcium deposits, known as microcalcifications. These microcalcifications are often too small to be detected by ultrasound but are easily seen on a mammogram.
Ultrasound is most effective as a targeted diagnostic tool rather than a general screening method. When a specific area of concern is identified—whether through another imaging test or a clinical breast exam—ultrasound provides additional clarity. It helps radiologists better understand what they are seeing and aids in determining whether further imaging or biopsy is needed. It is also valuable for women with dense breast tissue, where mammograms may be more difficult to interpret.
Despite its limitations as a standalone screening tool, ultrasound plays a crucial role when used alongside other imaging methods. When combined with mammography, thermography, or MRI, it contributes another essential piece of the puzzle, helping create a more complete and accurate assessment of breast health.
MRI
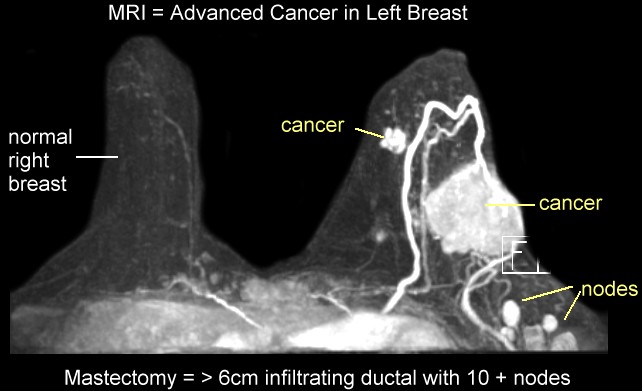
Magnetic resonance imaging (MRI) of the breast—commonly called a breast MRI—is an advanced imaging test used to detect breast cancer and identify other structural abnormalities within the breast tissue. Unlike mammograms or X-rays, which use radiation, an MRI relies on a powerful magnetic field and carefully calibrated radio waves to create highly detailed images. During the exam, the MRI machine captures multiple sets of images from various angles. A computer then processes these images and assembles them into precise, layered, three-dimensional views of the breast. This high level of detail makes MRI one of the most sensitive breast-imaging tools available.
Breast MRI is often performed after a biopsy confirms cancer. In this situation, the goal is not simply to detect the presence of disease but to determine its size, depth, and possible spread within the breast. MRI can reveal additional areas of concern that may not be visible on mammography or ultrasound, helping doctors plan surgery, evaluate treatment options, or determine whether cancer is present in more than one area of the breast.
For certain individuals, breast MRI may also be used as part of routine screening. This typically applies to women who are considered high-risk due to genetic factors, such as carrying a BRCA1 or BRCA2 mutation, or those with a strong family history of breast cancer. In these cases, MRI is often paired with mammography because the combination improves the chances of detecting cancer at the earliest possible stage.
Despite its strengths, MRI is not recommended for everyone as a general screening tool. It is more expensive, less accessible, and more sensitive—meaning it may detect benign findings that lead to additional testing or biopsies. It also requires the injection of contrast dye, which some individuals may not tolerate well.
Still, when used appropriately, breast MRI provides unmatched clarity and is an invaluable tool in both diagnosis and treatment planning. When combined with mammography, ultrasound, or thermography, it adds another essential layer of understanding to a woman’s breast-health strategy.
Summary
We strongly encourage you to have an open, informed conversation with your doctor about which breast-screening method—or combination of methods—is best for your individual needs. Every woman’s body, history, and risk factors are unique. Because of that, no single imaging test is capable of providing a complete picture of breast health on its own. Modern medical science overwhelmingly supports the view that the most accurate, reliable approach comes from using multiple complementary screening tools rather than relying exclusively on just one.
Each method of breast imaging comes with its own distinct strengths, limitations, and areas where it performs best. Mammography remains the FDA-recommended starting point for breast screening because it is excellent at identifying certain structural changes, such as calcifications. However, it does not capture physiologic change, and its accuracy decreases for women with dense breast tissue. Thermography excels at detecting early physiologic changes—such as inflammation, abnormal vascular activity, or metabolic heat patterns—that often emerge long before structural abnormalities appear. Yet thermography does not replace mammograms or ultrasounds, because it does not visualize anatomy.
Ultrasound is extremely useful for clarifying the nature of lumps and distinguishing solid from fluid-filled structures, but it is not reliable for detecting early calcifications. MRI offers outstanding detail and high sensitivity, but it is expensive, not suitable for everyone, and often reserved for high-risk cases or post-diagnosis evaluation. These differences highlight why no single test can serve as the sole authority on breast health.
It is also important to remember that every screening tool—no matter how advanced—has the potential for false positives and false negatives. This is not a flaw of the technology; it is simply the nature of medical imaging. Each test sees the breast through a different lens, revealing one unique layer of information while potentially missing another. In other words, every method has blind spots. Some are blind to early physiologic change. Others are blind to micro-calcifications. Some see structure beautifully but cannot detect inflammation. Others detect blood-flow changes but offer no insight into anatomical detail.
These limitations do not make any test “bad.” They simply mean that each test is specialized, with a defined scope. Understanding those scopes—and how they work together—is the key to creating an effective, personalized breast-health plan.
It is equally important to consider the potential risks associated with certain screening methods. Radiation exposure, repeated compression, contrast dyes, or the stress of false alarms can all impact your health in different ways. While these risks vary in magnitude, they should not be dismissed. They deserve thoughtful discussion with your healthcare provider so you can weigh the benefits of detection against the potential drawbacks of each approach.
Ultimately, the best path forward is a balanced, customized screening strategy—a package of complementary tests selected not out of fear or obligation, but out of informed confidence. When physiologic imaging, structural imaging, and clinical evaluation work together, they create the most complete, accurate, and empowering picture of breast health. This holistic approach supports earlier detection, stronger prevention, and more proactive long-term wellness.
Frequently Asked Questions
- If I receive a normal result from one screening (say a mammogram or thermogram), should I skip the other one until next year?
- How should I interpret a finding of increased vascular/thermal activity on a thermogram if my mammogram was normal?
- What lifestyle or baseline-health changes can I do alongside these screenings to improve my breast-health picture (so the testing is more meaningful)
Q1. “If I receive a normal result from one screening (say a mammogram or thermogram), should I skip the other one until next year?”
Answer: Not necessarily. A “normal” result from one type of screening is good, but it doesn’t guarantee that the other modalities have nothing to reveal. For example, as the blog explains, a mammogram (structure-based) may not pick up changes a thermogram (physiology-based) detects, and vice versa. If you have risk factors (family history, dense breast tissue, prior abnormal findings), using complementary modalities may give a more complete picture. Discuss with your physician whether combining screenings now (rather than waiting) makes sense for your individual profile.
Q2. “How should I interpret a finding of increased vascular/thermal activity on a thermogram if my mammogram was normal?”
Answer: Increased vascular or thermal activity on a thermogram may signal physiologic change (inflammation, lymphatic congestion, hormonal imbalance) rather than a structural mass that shows up on a mammogram.
While this doesn’t mean there is definitely cancer, it is a flag that warrants follow-up: either closer monitoring, lifestyle interventions (nutrition, hormone balance, lymphatic support), or structural imaging/diagnostic workup (ultrasound, MRI, mammogram) if clinically indicated. It’s important that the thermogram finding be correlated with your full clinical picture—symptoms, risk levels, physical exam and imaging history.
Q3. “What lifestyle or baseline-health changes can I do alongside these screenings to improve my breast-health picture (so the testing is more meaningful)?”
Answer: Good question — the screenings give valuable data, but what you do between scans can significantly impact what they show in future and your overall risk. Some ideas:
-
Use the thermogram baseline (if you had one) as a “starting line” and strive for decreased inflammatory markers, improved hormonal balance, better lymphatic drainage. For example, reduce chronic inflammation via diet (whole foods, reduce processed sugars), support exercise and maintain a healthy weight.
-
If you have dense breast tissue (which affects mammogram sensitivity) use strategies to reduce modifiable risk: manage estrogen exposure (via lifestyle, weight, medications if prescribed), reduce alcohol, quit smoking, ensure adequate physical activity.
-
Keep consistent documentation and baseline imaging—if you have a thermogram showing a “normal baseline,” periodic re-scans can help detect changes early.
-
Communicate with your doctor that you are using more than one modality (thermography + mammography/ultrasound) and ask for a coordinated screening plan tailored to you (age, risk, breast density, personal/family history).
By doing these things you enhance the context for the screenings so that when you revisit them (annual or biannual), you’re more than just reacting—you’re proactively improving the health environment these tests monitor.